- Children and Young Adults
- Engagement in Care
- Engagement in Research
- HIPxChange
- Quality and Safety
- Stakeholder Engagement
- Systems Engineering
Development of the toolkit
The FCR Toolkit was developed by a multidisciplinary group of family representatives, pediatric healthcare professionals at the American Family Children’s Hospital, and human factors and systems engineering researchers at the University of Wisconsin-Madison in the context of the Agency for Healthcare Research and Quality (AHRQ)-funded FCR Quality Improvement Initiative. The FCR Initiative aimed to increase family engagement in rounds for hospitalized children.
From a human factors and systems engineering viewpoint (Carayon et al., 2006; Carayon et al., 2014), the FCR checklist, by itself, is a tool. In order for the checklist to produce positive outcomes, it needs to be designed for and implemented in a large work system that involves multiple physicians, nurses, pharmacists, learners, parents and children who perform multiple tasks in a physical and organizational environment. This requires a thorough analysis of the current process of FCR and identification and prioritization of candidate strategies for improving family engagement, both of which provided input into the design of the intervention.
Implementation principles
In order to implement and institutionalize the FCR checklist intervention, research on human factors and ergonomics, quality improvement, and organizational change suggests that several key implementation principles need to be considered (Carayon et al., 2012; Karsh, 2004):
- Strong leadership support and commitment. The involvement of key leaders in the change process, which translates into visible actions (e.g., attendance at advisory meetings, talking about the FCR checklist whenever opportune) as well as allocation of resources, is critical for the implementation and sustainability of the intervention. In our case, a Steering Committee of leadership stakeholders was convened quarterly.
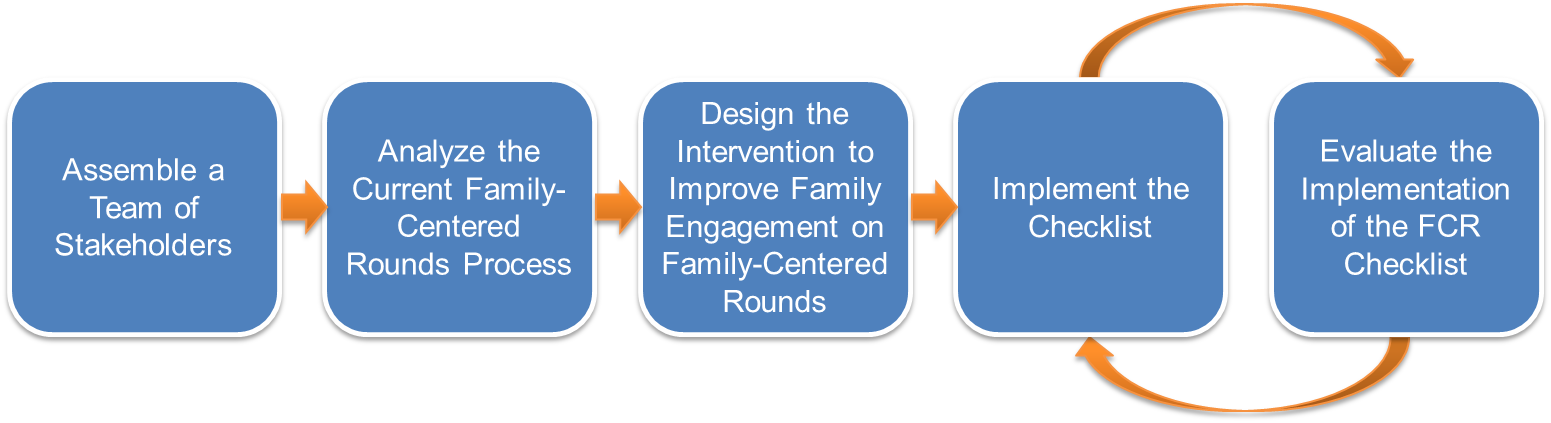
- An implementation plan and timeline. A process needs to be organized, structured and managed for the implementation. Our timeline summarizes the four phases of the project, including analysis of the FCR process, design of the FCR checklist intervention, implementation of the intervention, and evaluation of its implementation.
- Stakeholder participation. Active participation of "end users" or representative rounding stakeholders in the change process is a major factor of success. Our group of FCR stakeholders, the Intervention Implementation Team (IIT), was formed as a working group to: (1) define an intervention to enhance family engagement in FCR, (2) create an implementation plan for the intervention, (3) champion the implementation of the intervention, and (4) monitor and continuously improve the implementation.
- Multidisciplinary training. A major part of the integration of the FCR checklist into the rest of the work system is to provide people an opportunity to learn and practice the new behaviors. Therefore, we implemented a series of training and information sessions targeted at various stakeholder groups.
- Continuous evaluation and improvement. A scheme for continuously and periodically evaluating the implementation of the FCR checklist is necessary to provide feedback and ensure sustainability. We, therefore, developed several methods for evaluating the implementation of the FCR checklist, including an observation method aimed at examining the use of the FCR checklist during rounds.
Project team
We would like to thank all of the people who contributed to this project:
FCRI Steering Committee Members
- Linda A. Buel, MPH, AFCH Program Manager of Quality Resources, University of Wisconsin Hospital and Clinics
- Barb J. Byrne, DNP, AFCH Director of Pediatric Nursing, University of Wisconsin Hospital and Clinics
- Pascale Carayon, PhD, Procter & Gamble Bascom Professor of Industrial and Systems Engineering, Director of the Center for Quality and Productivity Improvement, UW-Madison
- Elizabeth D. Cox, MD, PhD, Principal Investigator, Associate Professor of Pediatrics, University of Wisconsin School of Medicine and Public Health
- Jon E. Fliegel, MD, Director of Hospitalist Service, Associate Professor of Pediatrics, University of Wisconsin School of Medicine and Public Health
- Martha (Meg) E. Gaines, JD. Associate Dean of Academic Affairs and Experiential Learning, Director of Center for Patient Partnerships (CPP), University of Wisconsin Law School
- Christopher G. Green, MD, AFCH Director of Quality and Professor of Pediatrics, University of Wisconsin School of Medicine and Public Health
- Diane G. Heatley, MD, AFCH Medical Director and Professor of Surgery, University of Wisconsin School of Medicine and Public Health
- Michelle Kelly, MD, Physician Champion, Assistant Professor of Pediatrics, Division of Hospital Medicine, University of Wisconsin School of Medicine and Public Health
- Gwenevere (Gwen) C. McIntosh, MD, MPH, Pediatric Residency Director and Vice Chair of Education, Associate Professor of Pediatrics, University of Wisconsin School of Medicine and Public Health
- Ellen R. Wald, MD, Professor and Chair of Pediatrics, University of Wisconsin School of Medicine and Public Health
Core Planning Group Members
- Roger L. Brown, PhD, Professor of Research Design & Statistics, University of Wisconsin School of Nursing
- Pascale Carayon, PhD, Procter & Gamble Bascom Professor of Industrial and Systems Engineering, Director of the Center for Quality and Productivity Improvement, UW-Madison
- Elizabeth D. Cox, MD, PhD, Principal Investigator, Associate Professor of Pediatrics, University of Wisconsin School of Medicine and Public Health
- Lori L. DuBenske, PhD, Clinical Health Psychologist, University of Wisconsin School of Medicine and Public Health
- Gwen Jacobsohn, PhD, Research Coordinator, University of Wisconsin School of Medicine and Public Health
- Michelle Kelly, MD, Physician Champion, Assistant Professor of Pediatrics, University of Wisconsin School of Medicine and Public Health
- Tosha Wetterneck, MD, MS, Associate Professor of Medicine, University of Wisconsin School of Medicine and Public Health
Writing Group Members
- Brenna C. McCabe, BS, Associate Research Specialist of Pediatrics, University of Wisconsin School of Medicine and Public Health
- Bryan H. Fate, BS, Student Research Assistant of Pediatrics, University of Wisconsin School of Medicine and Public Health
- Jason R. Orne, MS, BA, PhD Candidate of Sociology, University of Wisconsin-Madison
IIT Members
- Laura Ahola, RN, Nurse manager, AFCH
- Carisa Baker, RN, Nurse manager, AFCH
- Betsy Bender-Roe, RN, Staff nurse, AFCH
- Pascale Carayon, PhD, Group Co-Leader, Procter & Gamble Bascom Professor of Industrial and Systems Engineering, Director of the Center for Quality and Productivity Improvement, UW-Madison
- Andrea Carberry, MD, Pediatric resident
- Randi Cartmill, MS, Researcher at the Center for Quality and Productivity Improvement at UW-Madison
- Carol Diamond, MD, Associate Professor of Pediatrics, Division of Hematology and Oncology, University of Wisconsin School of Medicine and Public Health
- Mary Ehlenbach, MD, Assistant Professor of Pediatrics, Division of Hospital Medicine, University of Wisconsin School of Medicine and Public Health
- Diane G. Heatley, MD, AFCH Medical Director and Professor of Surgery, University of Wisconsin School of Medicine and Public Health
- Michelle Kelly, MD, Group Co-Leader, Assistant Professor of Pediatrics, Division of Hospital Medicine, University of Wisconsin School of Medicine and Public Health
- Cathy Lee-Miller, MD, Pediatric chief resident
- Yaqiong Li, MS, Ph.D. student in Industrial and Systems Engineering and research assistant at the Center for Quality and Productivity Improvement at UW-Madison
- Julie Plotkin, JD, parent representative, member of AFCH Patient and Family Advisory Council
- Anping Xie, Ph.D., Ph.D. student in Industrial and Systems Engineering, research assistant at the Center for Quality and Productivity Improvement at UW-Madison
- Katy Zahm, RN, Staff nurse, AFCH
Project funding
This project was funded by an Agency for Healthcare Research and Quality Health Services (AHRQ) Research Dissemination and Demonstration grant, R18 HS018680 to Dr. Cox, and also supported by the Arthur Vining Davis Foundation and the National Patient Safety Foundation through the James S. Todd Memorial Research Award. Additional support was provided by the University of Wisconsin School of Medicine and Public Health’s Health Innovation Program (HIP) and the Community-Academic Partnerships core of the University of Wisconsin Institute for Clinical and Translational Research (UW ICTR), grant UL1TR000427 through the NIH National Center for Advancing Translational Sciences (NCATS) Clinical and Translational Science Award (CTSA). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or other funders.
Use of the toolkit
![]()
The Family-Centered Rounds Toolkit, available at https://hipxchange.org/familyrounds, is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
The Family-Centered Rounds Toolkit exists for the benefit of the health care community. These materials are available free of charge and can be used without permission; however, we ask that you register with HIPxChange prior to using the toolkit so that we may provide information on usage to our funders. It is acceptable to link to this Web site without express permission.
The details of the methodology and findings from a randomized trial of this toolkit are available in the following article:
Cox ED, Jacobsohn GC, Rajamanickam VP, Carayon P, Kelly MM, Wetterneck TB, Rathouz PJ, Brown RL. A Family-Centered Rounds Checklist, Family Engagement, and Patient Safety: A Randomized Trial. Pediatrics. 2017 May;139(5):e20161688.
If you use these materials, we ask that you please cite the above article as well as this toolkit. We suggest using the following citation for this toolkit:
Cox ED, Carayon P, Kelly M, DuBenske LL, Wetterneck TB, Brown RL."The Family-Centered Rounds Toolkit." Madison, WI: University of Wisconsin – Madison Department of Industrial and Systems Engineering, Department of Pediatrics, Institute for Clinical and Translational Research, and UW Health Innovation Program; 2014. Available at: https://hipxchange.org/familyrounds.

 What is the Family-Centered Rounds Toolkit?
What is the Family-Centered Rounds Toolkit?