*Free registration is required to use the toolkits provided within HIPxChange. This information is required by our funders and is used to determine the impact of the materials posted on the website.
A specialty staff protocol to improve referrals to tobacco quit lines
The Clinical Problem
Smoking is a known risk factor for developing chronic conditions such as rheumatoid arthritis (RA), hypertension, and lung disease and is a leading preventable cause of early mortality. Additionally, smoking can exacerbate chronic conditions and cause premature cardiovascular disease. For example, smoking is a predictor of severe, treatment-refractory disease in RA and other rheumatic conditions. However, unlike primary care, specialty clinics that treat many chronic disease patients do not systematically provide resources to help patients quit smoking.
Studies show that 70% of smokers consider quitting and 40% try each year. Having assistance, such as free tobacco quit line support, increases quit rates four-fold; however, 60% of patients do not have assistance, despite the availability of free telephone quit lines in every state.
Gap in Specialty Care
In a previous study, we reported that only 10% of notes from eligible RA clinic visits documented cessation counseling, and only one in 175 notes recommended quit line phone services. Quit line services are free in every state and recommended by US guidelines to improve quit rates, and the Ask-Advise-Connect model has been shown to increase the proportion of patients being referred to quit lines 13-fold. However, these resources are rarely leveraged in rheumatology or other specialty clinics, and the existing models used in primary care have not been tailored for use in specialty clinics.
Specialty clinic visits outnumbered primary care visits in the United States in 2013, and specialty physicians outnumber primary care physicians. As such, specialty clinics have the opportunity to improve smoking cessation rates for patients with chronic conditions.
The Solution
The Quit Connect intervention was created to address these issues.
Quit Connect is designed to connect patients who are identified as smokers in a specialty visit to a quit line so that they have a greater chance of succeeding at quitting smoking.
How was it developed?
The Quit Connect staff protocol was developed at three rheumatology clinics at a large academic health system.
We conducted a participatory work system redesign to develop the protocol and held two hour-long focus group sessions with medical assistants (MAs) and nurses to (a) assess current processes and needs, and (b) develop a proposed electronic health record-based quit line referral process.
Does it work?
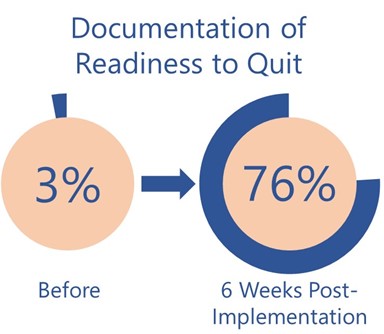 In the Quit Connect pilot study, at week 6, the protocol increased tobacco status documentation to 97%, documentation of 30-day readiness to quit increased from 3% to 76% and 32% of those asked reported readiness in the next 30 days.
In the Quit Connect pilot study, at week 6, the protocol increased tobacco status documentation to 97%, documentation of 30-day readiness to quit increased from 3% to 76% and 32% of those asked reported readiness in the next 30 days.
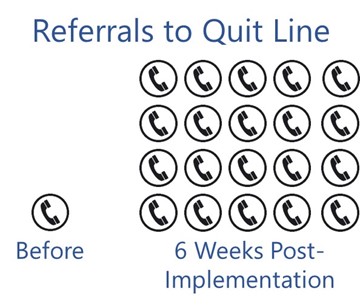
Overall, 12% of patients who smoked agreed to the quit line electronic referral versus 0.6% being offered the referral prior to the intervention—a 20-fold increase in quit line referrals.
What are people saying about the toolkit?
“The way you championed, built, and tested Wisconsin Tobacco Quit Line eReferral in Rheumatology was impressive. The fact that Wisconsin Tobacco Quit Line eReferral then spread throughout UW Health outpatient and then to UW Hospital inpatient has made a huge impact in the number of patients who use tobacco and have gotten referred to cessation services.” – Rob Adsit, MEd, Director of Education and Outreach, CTRI
About the Quit Connect toolkit
This toolkit contains the following materials:
- Quit Connect Manual (this document)
- Overview Slides on the Intervention: An overview of the importance of smoking cessation support and the Quit Connect protocol that can be used to present to health system leadership, physicians, staff, and other stakeholders
- EHR Build Guide: A guide to building the appropriate Quit Connect alerts and interface orders in the electronic health record
- Training Slides for Staff: A PowerPoint that can be used to educate staff on smoking cessation, why it is important, and the Quit Connect protocol
- Training Handout for Staff: Handout for role-play/scenario training with medical assistants and nurses
- Medical Assistant/Nurse Instructions: Instructions for medical assistants and nurses on how to follow the Quit Connect protocol that are meant to be laminated and placed in clinic rooms as quick references
- Patient Brochure: A brochure that nurses or medical assistants can give to patients when tobacco use is identified
Who should use this toolkit?
This toolkit is intended for health care administrators, clinicians, and/or researchers who seek to improve smoking cessation care and referrals to tobacco quit lines or other tobacco support resources from specialty clinics.
While the original implementation of Quit Connect was in rheumatology clinics, it could also be used in other specialty clinics.
Development of this toolkit
The Quit Connect Toolkit was developed by a multidisciplinary team of researchers and clinicians at the University of Wisconsin-Madison.
Christie Bartels, MD, MS, (principal investigator), School of Medicine & Public Health, Department of Medicine, Rheumatology Division
Edmond Ramly, PhD, Indiana University-Bloomington School of Public Health, Department of Health & Wellness Design
Daniel Panyard, PhD Candidate, School of Medicine & Public Health, Department of Population Health Sciences
Diane Lauver, PhD, RN, FNP, FAAN, School of Nursing
Heather M. Johnson, MD, MS, Baptist Health South Florida, Lynn Women’s Health & Wellness Institute
Kristin Steffen Lewicki, MD, School of Medicine & Public Health, Department of Medicine, General Internal Medicine Division
Patrick McBride, MD, MPH, FAHA, FACC, School of Medicine & Public Health, Department of Medicine, Cardiovascular Division, and Department of Family Medicine and Community Health
UW Center for Tobacco Research and Intervention (UW-CTRI), developers of the e-referral interface mechanism and co-creators of educational materials herein
UW Health
Funding
Portions of this project were supported in part by Independent Grants for Learning and Change (Pfizer) and by a grant collaboration from the University of Wisconsin (UW) Clinical and Translational Science Award (CTSA) and UW School of Medicine and Public Health’s Wisconsin Partnership Program, through the NIH National Center for Advancing Translational Sciences (NCATS grant UL1TR000427). Additional support was provided by the University of Wisconsin School of Medicine and Public Health’s Health Innovation Program (HIP). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or other funders. Please send questions, comments and suggestions to HIPxChange@hip.wisc.edu.
Quit Connect program highlighted by CDC, Million Hearts
Centers for Disease Control and Prevention. Tobacco Cessation Change Package. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services; 2020. (See Appendix B) https://www.cdc.gov/tobacco/basic_information/for-health-care-providers/clinical-tools/index.html
References
- Brandt J, Ramly E, Lim SS, Bao G, Messina ML, Piper ME, Bartels CM. Implementing a Staff-Led Smoking Cessation Intervention in a Diverse Safety-Net Rheumatology Clinic: a pre-post scalability study in a low resource setting. Arthritis Care Res (Hoboken). (in press)
- Ramly E, Lauver DR, Gilmore-Bykovskyi A, Bartels CM. Interactive and Participatory Audit and Feedback (IPAF): theory-based development and multi-site implementation outcomes with specialty clinic staff. Implement Sci Commun. 2021 May 31;2(1):58.
- Wattiaux A, Bettendorf B, Block L, Gilmore-Bykovskyi A, Ramly E, Piper ME, Rosenthal A, Sadusky J, Cox E, Chewning B, Bartels CM. Patient Perspectives on Smoking Cessation and Interventions in Rheumatology Clinics. Arthritis Care Res (Hoboken). 2020 Mar;72(3):369-377.
- Bartels CM, Johnson L, Ramly E, Panyard DJ, Gilmore-Bykovskyi A, Johnson HM, McBride P, Li Z, Sampene E, Lauver DR, Lewicki K, Piper ME. Impact of a Rheumatology Clinic Protocol on Tobacco Cessation Quit Line Referrals. Arthritis Care Res (Hoboken). 2022 Sep;74(9):1421-1429.
- Panyard DJ, Ramly E, Dean SM, Bartels CM. Bridging clinical researcher perceptions and health IT realities: A case study of stakeholder creep. Int J Med Inform. 2018 Feb;110:19-24.
Toolkit Citation
Bartels CM, Ramly E, Panyard D, Lauver D, Johnson HM, Steffen Lewicki K, McBride P. “Quit Connect Toolkit.” University of Wisconsin – Madison School of Medicine and Public Health, UW Center for Tobacco Research and Intervention, and UW Health. Madison, WI; 2017. Available at: https://www.hipxchange.org/QuitConnect.