- Chronic Conditions
- Dissemination and Implementation
- HIPxChange
- Hypertension
- Prevention
- Quality and Safety
*Free registration is required to use the toolkits provided within HIPxChange. This information is required by our funders and is used to determine the impact of the materials posted on the website.
A specialty staff protocol to improve follow-up after high blood pressures
The Clinical Problem
High blood pressures are one of the most prevalent and reversible cardiovascular disease risk factors among adults with chronic conditions, who are often vulnerable to gaps between specialty and primary care. Increasing preventive services to address hypertension could prevent more early deaths than any other preventive service, such as lipid treatment, cancer screening, and pneumococcal or influenza vaccination.
“There is nothing that will save more lives than controlling blood pressure.”
– Former CDC Director
Gap in Specialty Care
It is rare that high blood pressure is addressed in specialty visits. For example, in rheumatology visits where a blood pressure of ≥160/100 was taken,
- blood pressure was not discussed/documented in two-thirds of the visits, and
- only 1 in 10 received any advice to follow-up for high blood pressure.
This may be due, in part, to the perception that specialists do not consider blood pressure care to be within the purview of their practice.
Specialty clinic visits outnumber primary care visits in the United States, and specialty physicians outnumber primary care physicians. As such, specialty clinics have the opportunity to improve cardiovascular care for patients most at risk.
The Solution
To address these issues, the BP Connect staff protocol was created from an evidence-based primary care hypertension staff protocol, which was adapted for use in specialty clinics.
BP Connect is designed to connect patients with high blood pressure in a specialty visit back to primary care for timely follow-up.
It is a staff protocol performed by nurses or medical assistants during vitals assessment using electronic health record (EHR) alerts, brief counseling, and a simple clickable follow-up order. The short video below explains the protocol.
BEFORE: “There is no system. I don’t ever know what happens.”
– Rheumatology MAAFTER: “You just have so many high ones… it would just be, ‘Oh, it’s always like that.’ Once you get used to doing [the protocol], it’s actually easier.”
– Rheumatology MA
How was it developed?
The BP Connect staff protocol was developed at three rheumatology clinics at a large academic health system.
We conducted a participatory work system redesign to develop the protocol, and held two hour-long focus group sessions with medical assistants (MAs) and nurses to (a) assess current processes and needs, and (b) develop a proposed electronic health record-based blood pressure alert and referral process.
Does it work?
BP Connect implementation DOUBLED the number of timely primary care follow-up visits after specialty visits with high blood pressures.
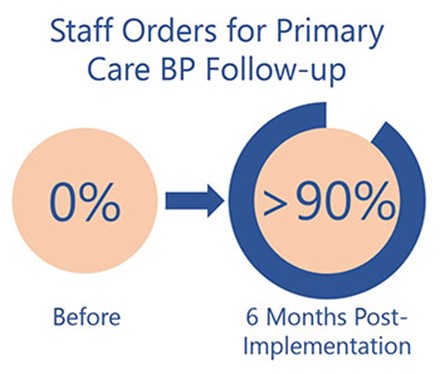 Additionally, in the BP Connect pilot study, the protocol increased blood pressure re-measurement from 2% to over 75% and staff orders for primary care follow-up improved from 0% to 76% averaged over the 6-month pilot, with a peak of >90% near the completion of the study.
Additionally, in the BP Connect pilot study, the protocol increased blood pressure re-measurement from 2% to over 75% and staff orders for primary care follow-up improved from 0% to 76% averaged over the 6-month pilot, with a peak of >90% near the completion of the study.
Staff members who said that they were very or extremely confident in dealing with high blood pressure increased from 20% to 90%.
About the BP Connect toolkit
This toolkit contains the following materials:
- BP Connect Manual: Information on how to implement the BP Connect protocol
- Overview Slides on the Intervention: An overview of the importance of hypertension preventive care and the BP Connect program that can be used to present to health system leadership, physicians, staff, and other stakeholders
- EHR Build Guide: A guide to building the appropriate BP Connect alerts in the electronic health record
- Training Slides for Staff: A PowerPoint that can be used to educate staff on hypertension, why it is important, taking an accurate blood pressure reading, and the BP Connect staff protocol
- Training Handouts for Staff: Handouts for role play/scenario training with medical assistants and nurses, along with accompanying talking points
- Medical Assistant/Nurse Instructions: Instructions for medical assistants and nurses on how to follow the BP Connect staff protocol that are meant to be laminated and placed in clinic rooms
- Scheduler Instructions: Instructions for schedulers on how to schedule follow-up appointments and guidance on answering common patient questions; intended to be laminated and kept at scheduler desks
- Patient Brochure: A brochure that nurses, medical assistants, or schedulers can give to patients when high blood pressure is identified
- Time-study Observation Tool: A tool that can be used to measure the time the rooming process takes before and after the implementation of BP Connect
Who should use this toolkit?
This toolkit is intended for health care administrators, clinicians, and/or researchers who seek to improve follow-up care when high blood pressure is identified in specialty clinics.
While the original implementation of BP Connect was in rheumatology clinics, it could also be used in other specialty clinics. The program would be particularly relevant to specialties associated with high cardiovascular disease risk (e.g., status post-cancer, HIV care, etc) where high blood pressures are not addressed routinely (e.g., not cardiolovascular specialty clinics).
Development of this toolkit
The BP Connect Toolkit was developed by a multidisciplinary team of researchers and clinicians at the University of Wisconsin-Madison.
Christie Bartels, MD, MS, (principal investigator), School of Medicine & Public Health, Department of Medicine, Rheumatology Division
Edmond Ramly, PhD, Center for Health Systems Research & Analysis, Department of Industrial & Systems Engineering, and Department of Medicine
Danny Panyard, PhD Candidate, School of Medicine & Public Health, Department of Population Health Sciences
Diane Lauver, PhD, RN, FNP, FAAN, School of Nursing
Heather M. Johnson, MD, MS, School of Medicine & Public Health, Department of Medicine, Cardiovascular Division
Kristin Steffen Lewicki, MD, School of Medicine & Public Health, Department of Medicine, General Internal Medicine Division
Patrick McBride, MD, MPH, FAHA, FACC, School of Medicine & Public Health, Department of Medicine, Cardiovascular Division, and Department of Family Medicine and Community Health
Funding
Portions of this project were supported in part by Independent Grants for Learning and Change (Pfizer) and by a grant collaboration from the University of Wisconsin (UW) Clinical and Translational Science Award (CTSA) and UW School of Medicine and Public Health’s Wisconsin Partnership Program, through the NIH National Center for Advancing Translational Sciences (NCATS grant UL1TR000427). Additional support was provided by the University of Wisconsin School of Medicine and Public Health’s Health Innovation Program (HIP). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or other funders.
Please send questions, comments and suggestions to HIPxChange@hip.wisc.edu
References
- Ramly E, Lauver DR, Gilmore-Bykovskyi A, Bartels CM. Interactive and Participatory Audit and Feedback (IPAF): theory-based development and multi-site implementation outcomes with specialty clinic staff. Implement Sci Commun. 2021 May 31;2(1):58.
- Bartels CM, Ramly E, Johnson HM, Lauver DR, Panyard DJ, Li Z, Sampene E, Lewicki K, McBride PE. Connecting Rheumatology Patients to Primary Care for High Blood Pressure: Specialty Clinic Protocol Improves Follow-up and Population Blood Pressures. Arthritis Care Res (Hoboken). 2019 Apr;71(4):461-470.
- Ramly E, Stroik B, Lauver DR, Johnson HM, McBride P, Steffen Lewicki K, Arnason J, Bartels CM. Assessing Unwanted Variations in Rheumatology Clinic Previsit Rooming. J Clin Rheumatol. 2019 Apr;25(3):e1-e7.
Toolkit Citation
Bartels CM, Ramly E, Panyard D, Lauver D, Johnson HM, Steffen Lewicki K, McBride P. “BP Connect Toolkit.” University of Wisconsin – Madison School of Medicine and Public Health. Madison, WI; Updated 2020. Available at: https://www.hipxchange.org/BPConnectHealth.